Patients with diabetes are at a higher risk for developing eye conditions because uncontrolled sugar levels can weaken blood vessels in the eye. Over 40 percent of patients diagnosed with diabetes develop some form of eye disease. When blood vessels are weakened, blood or fluid can leak from the blood vessels into the retina. In addition, new and fragile blood vessels can also start to grow in the retina. As a result, the risk of vision loss is increased.
It is important for patients with diabetes to have dilated eye exams once a year to detect any signs of diabetic eye disease as soon as possible. You can also minimize your risk of developing diabetic eye disease by keeping your blood sugar and blood pressure under control, eating a healthy diet and exercising regularly.
Diabetic Retinopathy
Diabetic retinopathy is the most common diabetic eye disease and is a leading cause of blindness in adults. Diabetic retinopathy develops as a result of changes in blood sugar levels or simply the presence of long-term diabetes. Most patients don't develop this condition until they have had diabetes for at least 10 years.
Patients who develop diabetic retinopathy may not initially notice any changes to their vision. In its earliest stages, this condition causes tiny areas of swelling in the small blood vessels of the retina. As the disease progresses, more and more blood vessels can become damaged, and the retina may send signals for new and fragile blood vessels to grow. These new blood vessels are more prone to leaking and bleeding and will result in rapidly decreased vision if not treated.
The early stages of diabetic retinopathy do not usually require treatment, unless the changes are visually threatening. Careful monitoring of the retina is important in managing diabetic retinopathy. In more advanced stages of the disease, treatment is needed to prevent further loss in vision.

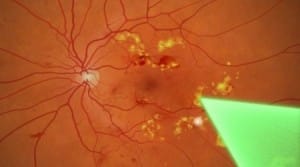
Proliferative Diabetic Retinopathy
Proliferative diabetic retinopathy, which is the most advanced stage of diabetic retinopathy, is classified by the growth of new and weakened blood vessels in the retina. These blood vessels are abnormal and fragile, and are susceptible to leaking blood and fluid in the retina, which can cause severe vision loss and even blindness.
If blood leaks into the vitreous, which is the gel-like fluid inside the eye that is in front of the retina, patients may begin to notice floaters in their vision. It is important to see your doctor as soon as you notice them, as they can lead to more permanent damage and vision loss.
Treatments for proliferative diabetic retinopathy include lasers and injections to slow down the growth of new blood vessels. In cases of severe bleeding, surgery is required to remove blood from inside the eye. Patients who have had extensive laser treatment may have slightly reduced color, night and/or peripheral vision; however, the treatment is important for preserving central vision.
Diabetic Macular Edema
Macular edema is a serious condition that can occur at any stage of diabetic retinopathy and involves a buildup of fluid in the macula, the light-sensitive part of the retina that allows us to see objects with great detail. Macular edema causes blurred vision at all distances, and can often greatly affect a patient's quality of life by interfering with regular activities.
Your doctor can diagnose macular edema during your regular eye exam before symptoms are present, but you should seek prompt medical attention at the earliest signs of this condition.
Treatment for macular edema usually includes a laser procedure called focal laser treatment. During this procedure, several hundred small laser burns are placed in the areas of retinal leakage around the macula to prevent leakage from occurring and reduce the amount of fluid in the retina. This helps reduce the risk of vision and can even improve vision in a small number of cases. Focal laser treatment is performed in the doctor's office and can usually be completed in just one session.

Diagnosing Diabetic Eye Conditions
Diabetic eye conditions can be detected through a comprehensive eye exam. A comprehensive eye exam does not only check visual acuity, but also involves a dilated eye exam to examine the structures of the eye for any signs of disease. The retina and optic nerve are examined using a special magnifying lens.
In a healthy eye, eye exams should be performed at least once a year. Early detection is the strongest protection against diabetic eye diseases.
Treatment of Diabetic Eye Conditions
Treatment for early stages of diabetic retinopathy and other conditions usually focuses on maintaining healthy and consistent levels of blood sugar, blood pressure and blood cholesterol to prevent any permanent damage from occurring. For patients with advanced cases, the following treatments may be needed:
Pan-Retinal Photocoagulation (PRP): This laser destroys abnormal blood vessel growth in patients with proliferative diabetic retinopathy. This procedure works best before the blood vessels have started to leak. The procedure can disrupt peripheral (side) vision, but will prevent further central vision loss. This treatment usually requires two or more sessions to fully treat the blood vessels. If there is blood in the eye obscuring the laser, a surgical procedure, also known as a vitrectomy, may be performed first to drain the blood in preparation for the laser.
Vitrectomy: The vitreous is the clear, gel-like substance that fills the center of the eye. The vitreous accounts for approximately two-thirds of the eye's volume, giving it its shape. Diseases or disorders of the vitreous may affect the vision since light may not be able to properly pass through the vitreous to reach the retina.
Patients with disease or injury to the vitreous may benefit from a vitrectomy. This surgery consists of the removal of the diseased vitreous from the eye and replacement of the displaced volume with air or gas as the eye heals. After removal of the vitreous, the doctor may treat the retina with a laser, cut or remove scar tissue, flatten detached areas of the retina, or repair holes or tears in the retina. Patients may experience mild discomfort and redness for several days after this procedure, and often will have their eye patched for the first day.
Although results vary depending on the individual condition treated, most patients experience improved visual acuity after this procedure. Vitrectomy is most effective in treating conditions such as a macular hole, retinal detachment, diabetic retinopathy, vitreous hemorrhage or an injury or infection in the vitreous.
Although this procedure is considered safe, there are certain risks associated with any surgical procedure. Some of these risks include retinal detachment, fluid buildup, growth of new blood vessels, infection and further bleeding into the vitreous gel.
Focal Laser: Macular edema, which is the swelling of the central retina called the macula, can be treated through a laser procedure called focal laser treatment. This treatment only requires one treatment.
Laser treatments can be performed in the doctor's office and are performed with anesthetic eye drops to minimize pain during the procedure. Patients may experience blurry vision for the rest of the day, and should rest at home. It is important for patients to realize that these procedures cannot cure diabetic eye conditions, but rather help reduce vision loss for patients with advanced cases of the condition.