Keratoconus
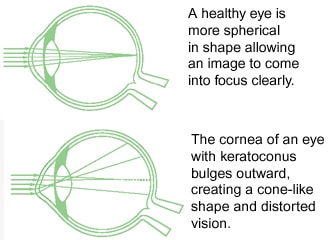
Keratoconus is a progressive eye disease in which the normally spherical cornea thins and begins to bulge into a cone-like shape. The cornea is a clear organ that lies in the central portion of the surface of the eye. In patients with keratoconus, the cone-shaped cornea cannot focus light rays properly and causes distorted vision.
Although many theories have been proposed, there is not one definite known cause of keratoconus. Possible etiologies include genetics, collagen deficiencies, and excessive eye-rubbing.
Signs and Symptoms of Keratoconus
Although keratoconus can develop at any age, it often begins to develop in the adolescent years to the early 20's. Changes in the shape of the cornea occur gradually, usually over several years. In most patients with keratoconus, both eyes will eventually be affected, though it is often more advanced in one eye compared to the other eye.
Keratoconus can be difficult to detect because it usually develops very slowly. Signs of keratoconus may include:
- Distorted and blurred vision
- Myopia (nearsightedness)
- Astigmatism
- Double vision
- Headaches due to eye strain
- Glare
- Light sensitivity
Your eye doctor will measure the curvature of your cornea to determine whether these symptoms are a result of keratoconus.
Treatment for Keratoconus
In the early stages of keratoconus, glasses or soft contact lenses may correct the nearsightedness and astigmatism associated with the disease. As the condition progresses and the cornea becomes increasingly thin, more advanced treatment is required. Treatment options include:
Rigid Gas-Permeable Contact Lenses, Scleral Lenses and Specialty Contact Lens Designs
If optimum vision is not achieved with eyeglasses or soft contact lenses, rigid gas-permeable (RGP) contact lenses, scleral lenses and specialty contact lens designs are used as a form of vision correction. The specialty lens covers the cornea and replaces the cornea's irregular shape with a smooth and uniform refracting surface. As a result, vision is improved.
The adaptation for wear-time of these specialty lenses varies depending on the type of lenses that are prescribed. The fitting process for these lenses take longer than the fitting process for conventional soft contact lenses as each person's cornea is unique. These lenses are designed to custom-fit your eye. If you are using specialty contact lenses, you will need to visit your doctor frequently to adjust the fit and prescription of the lenses as your keratoconus continues to progress.
Collagen Cross-Linking
Collagen cross-linking is a relatively new method for treating keratoconus. It works by strengthening the corneal tissue to slow down the thinning process. In this procedure, eye drops that contain riboflavin (vitamin B2) are applied to the cornea and then activated by ultraviolet light. This strengthens the collagen fibers within the cornea. Although approved in Europe, this procedure is undergoing FDA approval in the United States.
Corneal Transplant Surgery
Surgery is needed for patients with advanced keratoconus, especially if scarring has occurred. This treatment is usually recommended for 15-20% of cases. In corneal transplant surgery, most of the host cornea is removed and then replaced with a new donor cornea. The success rate of this procedure is over 97%.
Corneal Full Thickness Corneal Transplant (Penetrating Keratoplasty)
The cornea is the central clear portion in the front of the eye that bends and focuses light rays onto the retina in the back of the eye. A cornea that is scarred or swollen will lose its clarity and impede the proper transmission of light rays onto the retina, resulting in poor vision
A corneal transplant is recommended for a patient whose cornea is damaged due to disease, infection, or injury. Common indications for corneal transplantation include but are not limited to the following:
- Central corneal scars caused by keratoconus, chemical or mechanical injury, corneal ulcers, and herpes simplex virus keratitis
- Corneal edema (swelling)
- Corneal ulcers
- Corneal dystrophies
- Traumatic injury
Penetrating Keratoplasty Procedure
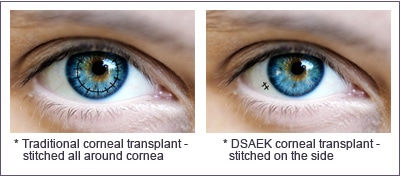
During the procedure, a circular incision is made into the cornea. A segment of the diseased corneal tissue is removed and replaced with healthy tissue that is sutured into place. Depending on the patient, local or general anesthesia may be used. The procedure time can range between 30-90 minutes.
A corneal transplant involves the replacement of the damaged cornea with a healthy donor cornea (obtained through an eye bank). There is a 90% success rate for full-thickness corneal transplants in patients with non-infectious causes.
Recovery and Risks of Penetrating Keratoplasty
Visual recovery may take from six to twelve months. Post-operative topical ocular medications are needed to prevent graft rejection and infection. Any discomfort or change in vision after the procedure should prompt a visit to your surgeon. Rejection, infection, and breaking of sutures may cause pain or discomfort that should be treated immediately.
Partial Corneal Transplant – Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK)
The cornea is the clear tissue that creates the front surface of the eye and focuses light rays onto the retina. For clear vision, the cornea must be smooth and clear. If the cornea becomes cloudy or distorted from injury, infection, or disease, a corneal transplant may be recommended.
There are several different corneal transplant procedures. The traditional full thickness corneal transplant procedure (penetrating keratoplasty) involves the replacement of the entire damaged cornea with a healthy cornea from a human donor tissue that is obtained from an eye bank. However, technological advances have allowed for the development of specialized procedures that replace only the damaged portion of the cornea, leaving the remainder of the cornea intact.
Descemet's Stripping and Automated Endothelial Keratoplasty (DSAEK) replaces only the innermost layers of the cornea. This allows the procedure to be performed through a much smaller incision with shorter recovery times and fewer risks than a traditional corneal transplant.
DSAEK is most commonly performed on patients with Fuchs' Dystrophy, an inherited eye disease in which the cells of the endothelium deteriorate, resulting in distorted vision and corneal swelling. As this condition progresses, the vision and comfort will worsen.
DSAEK Procedure
During the DSAEK procedure, a small incision is used to access the inner portion of the cornea and remove the damaged endothelial tissue. The donor endothelial tissue, which is prepared in the Eye Bank with a microkeratome blade, is then inserted into the eye. The donor tissue is then centered and held in place by an air bubble. The incision site is then closed with a few stitches. This procedure is performed with a topical anesthetic to minimize any potential discomfort and takes 30-45 minutes to perform.
Recovery from DSAEK
After the DSAEK procedure, patients will be moved to a recovery room for approximately two hours. Antibiotic and steroid eye drops will be prescribed. The first follow up appointment will be scheduled for the next day.
Many people will notice an improvement in their vision within the first few weeks after surgery. Vision usually continues to improve for the next three months. This is significantly faster than visual recovery after a traditional corneal transplant procedure, which may take six to twelve months. Those who experience a slower healing process may have had other existing eye conditions.
Risks of DSAEK
While the DSAEK procedure is relatively safe for most patients with corneal damage, there are risks similar to any other ocular surgical procedure, such as infection, bleeding, glaucoma, etc. Although rare, there is a risk of transplant rejection, which may result in redness, sensitivity to light and blurred vision. If these symptoms are experienced after DSAEK, a prompt visit to the eye doctor is important to prevent any permanent damage from occurring.