The cornea is the central clear portion in the front of the eye that bends and focuses light rays onto the retina in the back of the eye. A cornea that is scarred or swollen will lose its clarity and impede the proper transmission of light rays onto the retina, resulting in poor vision
A corneal transplant is recommended for a patient whose cornea is damaged due to disease, infection, or injury. Common indications for corneal transplantation include but are not limited to the following:
- Central corneal scars caused by keratoconus, chemical or mechanical injury, corneal ulcers, and herpes simplex virus keratitis
- Corneal edema (swelling)
- Corneal ulcers
- Corneal dystrophies
- Traumatic injury
A corneal transplant involves the replacement of the damaged cornea with a healthy donor cornea (obtained through an eye bank). There is a 90% success rate for full-thickness corneal transplants in patients with non-infectious causes.
Penetrating Keratoplasty Procedure
During the procedure, a circular incision is made into the cornea. A segment of the diseased corneal tissue is removed and replaced with healthy tissue that is sutured into place. Depending on the patient, local or general anesthesia may be used. The procedure time can range between 30-90 minutes.
Recovery and Risks of Penetrating Keratoplasty
Visual recovery may take from six to twelve months. Post-operative topical ocular medications are needed to prevent graft rejection and infection. Any discomfort or change in vision after the procedure should prompt a visit to your surgeon. Rejection, infection, and breaking of sutures may cause pain or discomfort that should be treated immediately.
Partial Corneal Transplant – Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK)
The cornea is the clear tissue that creates the front surface of the eye and focuses light rays onto the retina. For clear vision, the cornea must be smooth and clear. If the cornea becomes cloudy or distorted from injury, infection, or disease, a corneal transplant may be recommended.
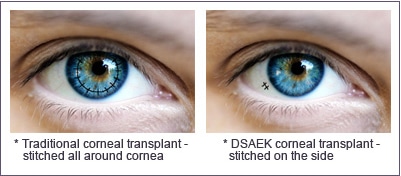
There are several different corneal transplant procedures. The traditional full thickness corneal transplant procedure (penetrating keratoplasty) involves the replacement of the entire damaged cornea with a healthy cornea from a human donor tissue that is obtained from an eye bank. However, technological advances have allowed for the development of specialized procedures that replace only the damaged portion of the cornea, leaving the remainder of the cornea intact.
Descemet's Stripping and Automated Endothelial Keratoplasty (DSAEK) replaces only the innermost layers of the cornea. This allows the procedure to be performed through a much smaller incision with shorter recovery times and fewer risks than a traditional corneal transplant.
DSAEK is most commonly performed on patients with Fuchs' Dystrophy, an inherited eye disease in which the cells of the endothelium deteriorate, resulting in distorted vision and corneal swelling. As this condition progresses, the vision and comfort will worsen.
DSAEK Procedure
During the DSAEK procedure, a small incision is used to access the inner portion of the cornea and remove the damaged endothelial tissue. The donor endothelial tissue, which is prepared in the Eye Bank with a microkeratome blade, is then inserted into the eye. The donor tissue is then centered and held in place by an air bubble. The incision site is then closed with a few stitches. This procedure is performed with a topical anesthetic to minimize any potential discomfort and takes 30-45 minutes to perform.
Recovery from DSAEK
After the DSAEK procedure, patients will be moved to a recovery room for approximately two hours. Antibiotic and steroid eye drops will be prescribed. The first follow up appointment will be scheduled for the next day.
Many people will notice an improvement in their vision within the first few weeks after surgery. Vision usually continues to improve for the next three months. This is significantly faster than visual recovery after a traditional corneal transplant procedure, which may take six to twelve months. Those who experience a slower healing process may have had other existing eye conditions.
Risks of DSAEK
While the DSAEK procedure is relatively safe for most patients with corneal damage, there are risks similar to any other ocular surgical procedure, such as infection, bleeding, glaucoma, etc. Although rare, there is a risk of transplant rejection, which may result in redness, sensitivity to light and blurred vision. If these symptoms are experienced after DSAEK, a prompt visit to the eye doctor is important to prevent any permanent damage from occurring.